"Don't screen everyone!": Rethinking spinal screening practices for shoulder pain
Article review of Requejo-Salinas et al., (2024)
Paper title and link to paper:
Neck or Shoulder? Establishing Consensus for Spine Screening in Patients with Shoulder Pain: an International Modified Delphi Study (Requejo-Salinas et al. 2024)
Overview:
I don’t think I can do a blog on looking at new shoulder pain research without discussing the following paper by Requejo-Salinas et al., (2024) which seems to have been flying around on social media at the moment. This paper builds on previous work such as that of Walker et al., (2020) who looked at what physiotherapists currently do in screening the neck in people with shoulder pain (which I have briefly discussed on an older blog post).
The current paper by Requejo-Salinas et al., (2024) aimed to develop some recommendations from experts in the physiotherapy field on how we should go about assessing the potential involvement of the spine when someone presents with shoulder pain. With a lack of consensus suggested in the literature, a Delphi study with three rounds was conducted in order to gain some clarity on this topic. The items for the study were drawn up by the working group which consisted of a literature review and a pilot study. Further suggestions on items were also made by the expert physiotherapists during the first round. These items were classified into either “Clinical reasoning”, “History”, or “Physical examination”. The experts were then tasked with determining their agreement of these statements using a five point likert scale, from strongly disagree to strongly agree.
The results were then analysed using the Aiken Validity Index (AVI) which gives an agreement coefficient from 0 to 1, with 1 suggesting perfect agreement. If an item was given a value of ≥ 0.7, the item was passed to the following round, and accepted if it passed the final round. I’ve not personally come across the AVI before but from reading the original paper by Aiken (1985), it seems to be a statistical method used for analysing data from validity ratings or judgements.
What did the experts recommend?
Initially, there were 148 items that the experts rated. After a round of voting, 62 items were passed into the second round. In the second round, 30 items made it through to the third round. In the final round of voting, all of these 30 items that passed the second round also reached consensus.
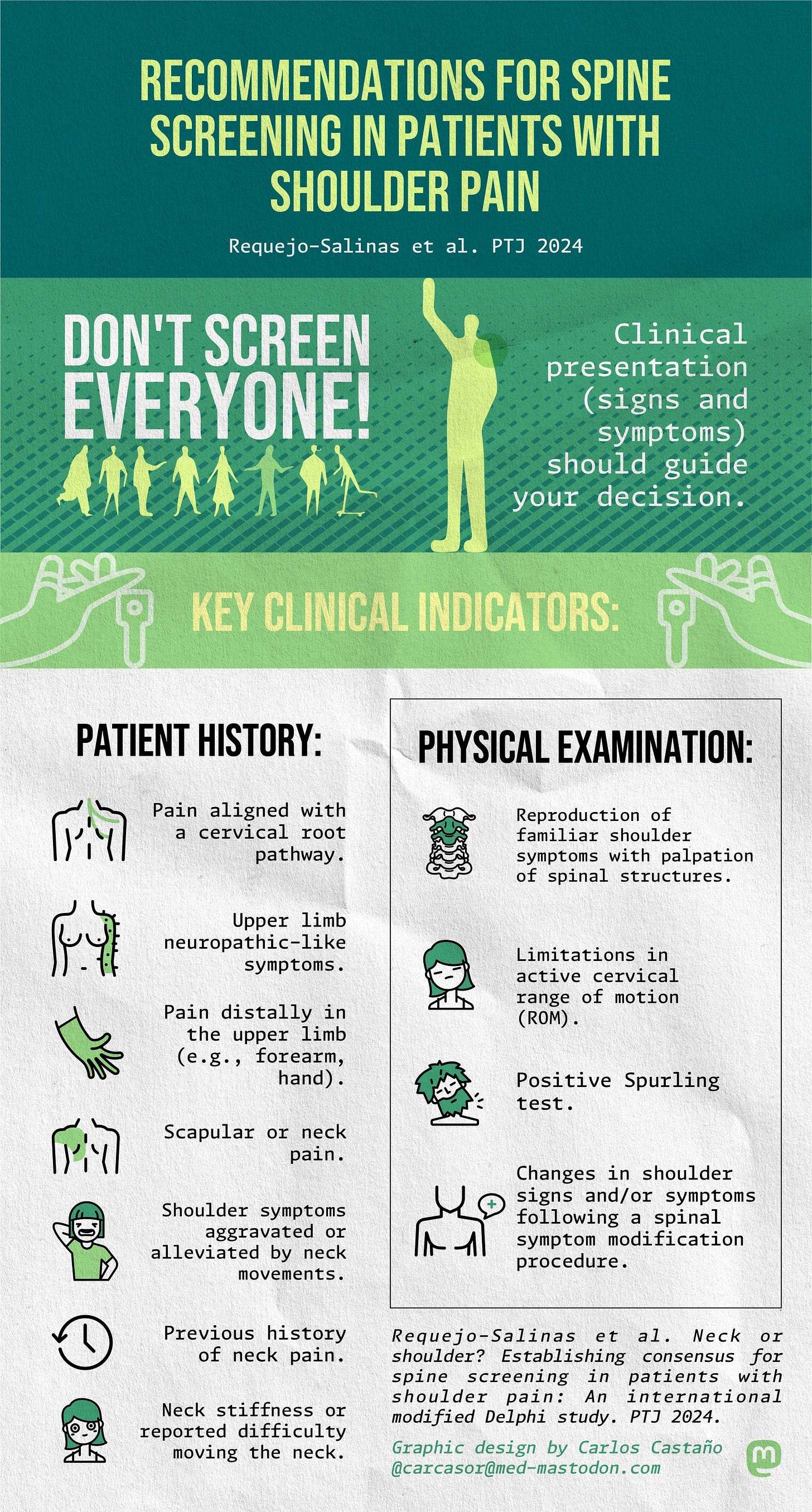
The infograph below, produced and included in the paper, gives you a summary of the recommendations given by the experts, and includes the phrase “Don’t screen everyone!”. This is a great snapshot and reference point to refer back to if we are seeing a patient with shoulder pain and we are questioning if they may have spinal involvement.
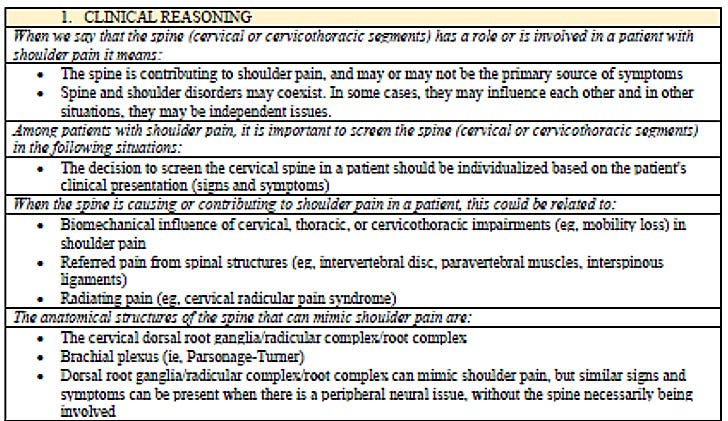
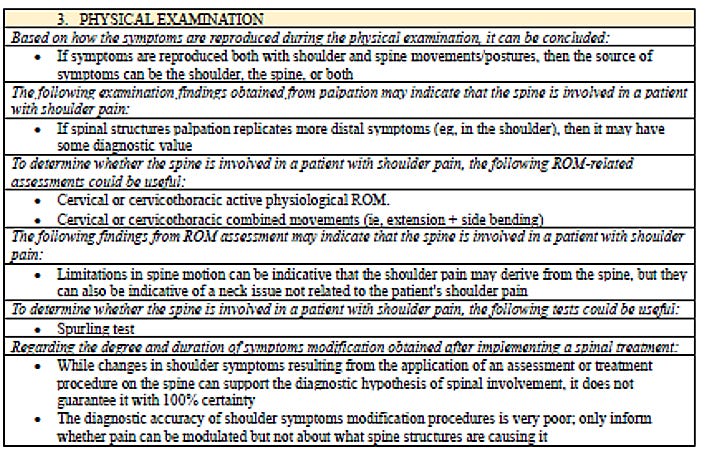
As someone who loves looking into the detail, I have also added the following tables from the paper of all 30 points that were agreed upon by the experts. This is broken down into three sections:
The clinical reasoning section
The subjective examination section
The physical examination section
“Don’t screen everyone”
One aspect that this paper really jumped out at me, and something that made me interested in looking at this study further was the words on the infograph of “Don’t screen everyone!”. In the full-text within the paper, the authors did however report on one item that did not reach the second round. This item was “The spine should be routinely screened in all shoulder pain presentations”. This achieved an Aiken value score of 0.69. As discussed above, an Aiken value of ≥ 0.7 would have passed this item onto the next round. So, this item was very close to getting through to the third round (where all of these items were then passed on for the final recommendations). I guess all I am highlighting here is the idea that this item was something which was agreed upon by a good majority of the experts but just didn’t quite make the threshold.
Why do I bring this up? Well, the necessity for screening the neck for everyone with shoulder pain is something that I have often have discussed with my peers in the past. I myself sit more in the camp of screening everyone. On reflection, I have probably been influenced in some way by the BOA/BESS patient care pathway infographic shown below in wanting to always screen the neck.
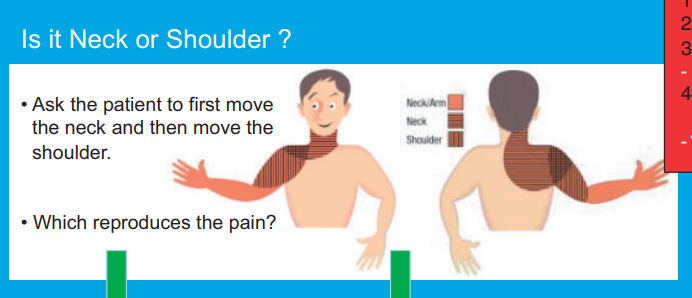
Following the findings of paper, this is something I feel I may need to reconsider in my own practice and screen on an individual, case by case approach, based on an individual’s presentation.
If you want to support me with my blog, buying me a coffee would help keep the motivation up!