My shoulder pain gets better when I put my hand on my head...
Overview of the Bakody's sign and article review of Walker et al., (2020)
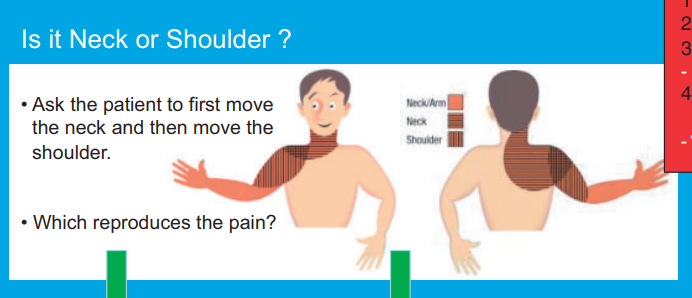
Is a patient’s problem their shoulder, or is it their neck? This is a conundrum that seemingly has no clear answer. A survey by Walker et al., (2020) on healthcare professionals, with the majority being physiotherapists, were given the following case study on a patient with shoulder pain:
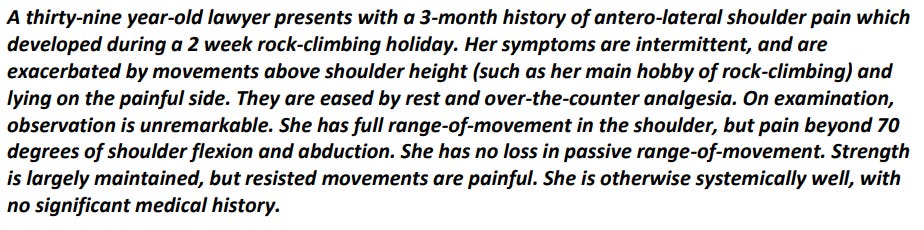
The participants were then asked whether they would assess the neck, and, if they did, how they would do it. Although over 80% of participants suggested they would assess the neck, there was large variability in what assessing the neck would involve. This ranged from strength testing (48.8%) to neurological examination (78.1%). Actively moving the neck was the most commonly suggested method of assessment (95.3%). This is in line with BESS/BOA patient care pathway guidelines, as shown below.
Walker et al., (2020) then questioned the healthcare practitioners on more details around this active movement assessment. This is where the details started to be not as decisive. The majority of participants stated they would do single movements (74%) with less participants suggested they would do repeated (53.6%), or combined movements (57.8%). A change in the patients’ symptoms (97.6%) was considered particularly important yet abnormal range of movement (69.3%) and quality of movement (46.9%) was also seen to be important to some participants when doing active cervical movement. So even the most simple method of asessment, actively moving the neck, has variability in practice.
What else can look out for?
During the subjective assessment, there are often times where one question or answer seems to steer the direction of assessment. Examples of this include when a patient reports a long smoking history, or, say if the patients starts to talk about their symptoms becoming bilateral. This makes me interested in the following sign which can also be used as a ‘test’.
The Bakody’s sign (Shoulder abduction relief test)
This ‘sign’ perks my interest whenever it comes up in the subjective as an easing factor. Quite simply, if you put your hand on your head and it relieves your symptoms, this is a positive finding. In the Walker et al., (2020) study discussed above, only 12.1% suggested they would use this ‘test’ for this case study. From my understanding from a talk by Roger Kerry, this test may be useful with patients who may be highly irritable, where something like a spurling’s test may be too provocative.
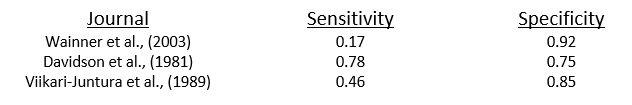
But how good is this test? Two systematic reviews (Rubinstein et al., 2007; Thoomes et al., 2018) have looked at tests for cervical radiculopathy. Only three journals have been cited, all of which are over 20 years old (Davidson et al., 1981; Viikari-Juntura et al., 1989; Wainner et al., 2003). This sensitivity and specificity within these papers are shown below.
On the whole, this test has poor sensitivity. If the patient’s symptoms are not relieved, we can’t really be clear that it is not from the neck. The specificity is slightly more promising. If the patient is relieved with this ‘test’, perhaps the neck, or even something more proximal to the neck (Kimura et al., 2023), is something we should be thinking about.
Can we rely on this test? No. Can this test, whether this to be an easing factor in the subjective or an objective test be useful toward considering neck related shoulder pain, I think so.
As always, if anyone has any comments, further reading or suggestions on this topic please feel free to fire them at me on here or on X. I am always learning, and any discussions would be thoroughly welcomed