What is "normal"? Normative data for active shoulder range of movement
Article review of Gill et al., (2020)
Paper title and link to paper:
Shoulder range of movement in the general population: age and gender stratified normative data using a community-based cohort (Gill et al., 2020)
Why this blog post may be useful to you:
Normative data on active range of movement in the shoulder to refer to
Diabetes vs. non-diabetes differences in active range of movement
Overview of the paper:
In rehabilitation of a shoulder injury, active range of movement may be one objective measure we seek to improve. The question is, what is a “normal” range of movement? We may have the contralateral limb that we could compare to, however, is comparing to a contralateral limb accurate? Textbook examples suggest blanket normal ranges of movement but does this really account for age or sex differences? The following paper helps to bridge this gap with normative data.
This study by Gill et al. (2022) uses participants recruited as part of the North West Adelaide Study (NWAHS). The NWAHS is a longitudinal cohort study which aims to create self-reported and measured data to help inform future policies around health care in the prevention of chronic diseases. Within this study, they took active range of movement measurements using an inclinometer in flexion, abduction, and external rotation (with hand by their side)
This study was based on people with no prior history of shoulder problems. Participants were excluded if they self-reported “yes” to the having had any history of:
“Shoulder pain or stiffness, or if they had ever been told by a doctor that they had rheumatoid arthritis”
This left 2404 participants with 711 (25.7%) participants being excluded.
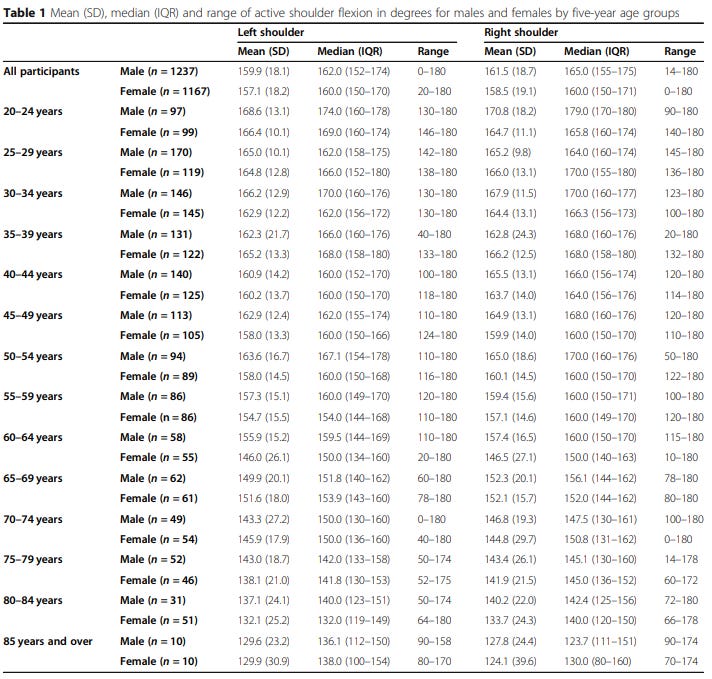
The following tables show the results of the three movements (flexion, abduction, and external rotation). They have split up the data by age and sex for left and right shoulder. Data is displayed using a mean, a median (with interquartile range) and a range (lowest to highest value).
Active shoulder flexion
Active shoulder abduction normative data
Active external rotation normative data
Range of movement targets
The above data gives us a rough guide to what active range of movement we should be aiming for. For example, if we are rehabilitating someone who is an 80 year female, a realistic target may be 115-120 degrees of shoulder flexion. This is opposed to a 20 year old female, where 115-120 degrees of shoulder flexion would be seen as something we may need to work on. I align this to other goals set on normative data such as the single calf raise strength test (Hébert-Losier et al., 2017) as used by Tom Goom for patients with lower limb problems.
Although improving objective measures such active range of movement may important, we have to remember that restoring full movement may not be necessary for people to return to functional activities of daily living. This can be said of the shoulder (Namdari et al., 2012) as well as other joints such as the elbow (Sardelli et al., 2011).
Exclusion criteria
If we first take it back to the exclusion criteria. The participants in the above data set self-reported they did not have any history of “shoulder pain or stiffness”.
When we look at the lowest value in the range (far right column), you will see that throughout the data sets, some participants have very low active range of movement scores as shown by the lowest number in the range. This is seen right through all three movements in both sexes. Some examples include:
Male (20-24 years old): Shoulder flexion - 90 degrees
Male (30-34 year old): Shoulder external rotation - 15 degrees
Female (40-44 years old): Shoulder abduction - 66 degrees
Female (60-64 years old): Shoulder flexion - 10 degrees
So, although as clinicians we could reason that these participants are “stiff” with low active range of movement scores, these participants feel (as self-reported) that they are problem free and “normal”. This highlights how varied the population is in regard to active range of movement and how an individual may perceived their health and function.
Range of movement in participants with diabetes
The authors also looked at active range of movement in those with and without diabetes. Those with diabetes had a statistically significantly active range of movement loss in all three directions analysed. This is something to consider if we are questioning any potential loss in movement in a patient with diabetes.
As always, if anyone has any comments, further reading or suggestions on this topic please feel free to fire them at me on here or on my Twitter. I am always learning and any discrepancies on what I have written is thoroughly encouraged.