Ultrasound following traumatic shoulder dislocation in the older age group
Article review of Zhou et al., 2021
Paper title and link to paper:
The significance of urgent ultrasound scan for shoulder dislocation in patients above the age of 40: A prospective British Elbow and Shoulder Society pathway implementation study (Zhou et al., 2021)
Overview of the paper:
In 2015, the British Elbow and Shoulder Society (BESS) and British Orthopaedic Association (BOA) published pathway guidelines on anterior traumatic shoulder instability (Brownson et al., 2015). These guidelines suggested in the summary that:
“Clinically relevant rotator cuff tears are present in at least 10% of patients. Patients over the age of 40 years should undergo investigation for this with a view to performing early rotator cuff repair to minimize functional loss”
This set the design for the study we are looking at by Zhou et al., (2021) who used this summary in clinical practice. Every patient above the age of 40 was given an urgent (within two weeks) ultrasound and were referred to a shoulder surgeon if a full-thickness rotator cuff tear (FRCT) was found.
The inclusion criteria for these patients was that they had to be over the age of 40, be the first time they have dislocated their shoulder, have no previous shoulder complaints and that they had radiological evidence of a glenohumeral joint dislocation.
54 patients met the criteria during the trial period. The authors’ documented the following about these patients:
10 patients required closed reduction in an operating theatre under general anaesthesia
18 patients sustained a greater tuberosity fracture
5 patients had a greater tuberosity fracture that had >5mm displacement pre-manipulation
3 patients had a greater tuberosity fracture that had >5mm displacement post-manipulation that required open reduction internal fixation (ORIF)
7 patients had neurological deficit (3 associated with the brachial plexus and 4 associated with the axillary nerve)
5 patients had recurrent dislocation within two weeks prior to any surgical intervention
3 patients had surgical management rather than continuing conservative care
Following exclusion of 14 out of 54 of the patients for reasons including mental health issues and for having medical problems unsuitable for surgery, 40 patient underwent USS.
Of these 40 patients, 23 had FRCTs. The supraspinatus was the most commonly tendon involved in all but one of the patients. Patients who were older, who had neurological deficit or those who had fatty infiltration in their tendons were more likely to have a FRCT.
The incidence of a FRCT in each age group were as followed:
40-50 years old - 1 out of 9 (11.1%)
50-60 years old - 1 out of 3 (33.3%)
60-70 years old - 7 out of 11 (63.6%)
70-80 years old - 10 out of 12 (83.3%)
80-90 years old - 4 out of 4 (100%)
These results need to be taken with caution, with some of the age group categories having very few patients in them which may under or overestimated the incidence of FRCT. For example, in the 50-60 years group there were just three patients with only one patient sustaining a FRCT thus making the incidence 33.3%. This can also be said with the 80-90 year old group where all four patients sustained a FRCT making the incidence 100%.
Of the 23 confirmed as having FRCT, 11 patients had surgery. These patients were on average younger (65 years old +/- 10.5) than those that did not have surgery (77 years old +/- 7.9). In those that that had surgery, the patients’ ages ranged from 47 to 77 years old.
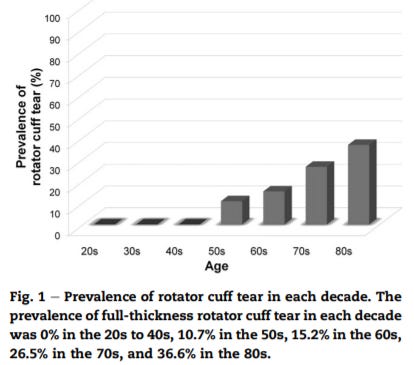
I feel this does somewhat open a can of worms as to know what we do from here. The patient now knows they have a FRCT, now what? We know that FRCT are not uncommon in an asymptomatic population especially with increasing age. This graph below is from a paper by Minagawa et al., (2013) which is commonly used in patient education to highlight the not so solid link between structural changes and pain.
Teunis et al., (2014) also looked at rotator cuff abnormalities in a systematic review and concluded “The prevalence of rotator cuff abnormalities in asymptomatic people is high enough for degeneration of the rotator cuff to be considered a common aspect of normal human aging and to make it difficult to determine when an abnormality is new (e.g., after a dislocation) or is the cause of symptoms.”
So if we take the four oldest patients who were between 80 and 90 years old, with the oldest being 89 years old. They all had a confirmed FRCT. Is this tear clinically relevant? Now we have told them a FRCT, what are we going to do about it? It is interesting to note that none of these had surgical repair.
I am fully aware that age does not necessarily represent health or tissue quality (Wroblewski et al., 2011) but should we really be blanket investigating everyone for a FRCT with an anterior dislocation over the age of 40?
I am not so convinced.
Key take away points:
USS may be helpful in picking up FRCT following a traumatic anterior shoulder dislocation
FRCT is not uncommon in traumatic anterior shoulder dislocation especially in the older population group
It is not clear how necessary it is to investigate everyone for a FRCT following a traumatic anterior shoulder dislocation in those over 40 years old
As always, if anyone has any comments, further reading or suggestions on this topic please feel free to fire them at me on here or on my Twitter. I am always learning and any discussions would be thoroughly welcomed