Nerve injury following a glenohumeral joint dislocation (with a focus on the Axillary nerve)
Article review of Avis and Power (2018) and Robinson et al., (2012)
Following a dislocation, an injury to the local nerves is an additional unwanted complication. In private practice last year, I had a few patients who had a glenohumeral dislocation with some signs of nerve pathology so I thought I would do some more reading around this area.
The British Elbow and Shoulder Society (BESS) and British Orthopaedic Association (BOA) patient care pathway (Brownson et al., 2015) summarised that following a traumatic anterior shoulder dislocation:
“Careful clinical examination should be performed to identify neurological injuries. Physiotherapy is essential in minimizing loss of movement in the presence of neurological injury. Electromyography (EMG) studies should be performed at 6 weeks if no clinical recovery is seen. Referral to a nerve injury centre is recommended if EMG studies at 6 weeks do not show evidence of recovery”
What does this careful clinical examination look like? This video series by surgeon Tom Quick has some brilliant videos on upper limb neurological assessment. He also has this video on nerve injury assessment which I have also found useful.
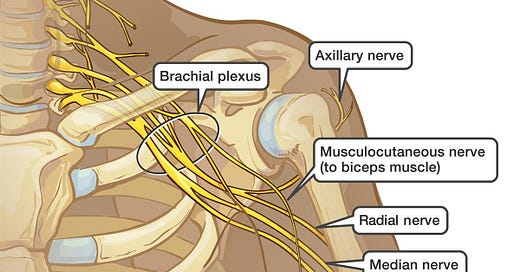
Furthering this, we can look at the nerves which may be more commonly affected. In a study based in an acute musculoskeletal trauma service in Edinburgh (Robinson et al., 2012), 13.5% of patients had evidence of a neurological deficit following an anterior shoulder dislocation. The most common peripheral nerve affected in this study population, as shown in the table below, was the axillary nerve (Robinson et al., 2012).
A paper by Avis and Power (2018) in EFORT open reviews looked at the axillary nerve in more detail. Here are some key areas discussed in the paper:
Anatomy of the Axillary nerve - Where does it goes and what does it innervate?
Part of the posterior cord arising from C5-T1
Passes through the quadrilateral space (see previous blog post on Quadrilateral space syndrome for anatomy)

Image taken from AboutKidsHealth Anterior branch innervates anterior, medial and (commonly) posterior deltoid
Posterior branch innervates posterior deltoid and teres minor
Posterior branch ends as the superior lateral brachial cutaneous nerve which innervates the proximal lateral arm
Management of Axillary nerve pathology
So, you think there is some sort of an injury to the Axillary nerve. Now what? Seddon and Sunderland created a classification system which may help to guide you with some ideas around the pathophysiology and subsequent recovery. As shown in the table below, the higher the grade, the more likely surgical intervention may be needed.

Axis and Power (2018) presented a simple treatment diagram for the axillary nerve in particular. It is worth checking on your local and/or national policy as this may likely differ from that shown below.

Who may have a poorer recovery?
And finally, we may also want to consider other factors which may impact recovery. Avis and Power (2018) suggested the following factors may be more likely to have a poorer outcome:
Increasing age of the patient
Presence of a fracture
Blunt trauma
Presence of a vascular injury
Longer time to reduction
Presence of other nerve injuries
Neuropathic pain (burning or deep aching)
As always, if anyone has any comments, further reading or suggestions on this topic please feel free to fire them at me on here or on my Twitter. I am always learning and any discrepancies on what I have written is thoroughly encouraged.